Summary
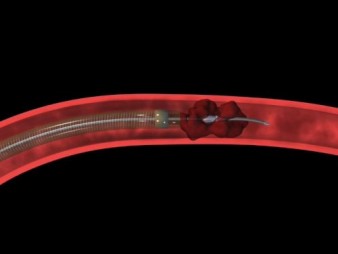
Similar concept also applies to brain attack. Vascular Neurosurgeon also prefers Percutaneous Cerebral Intervention (Neuro-PCI), rather than iv rtPA. The Neuro-PCI has to be performed within 8 hours after symptom onset. This is thus the new Golden-8-hours Concept for brain attack. Nowadays Neuro-PCI is the first line standard treatment offered by most Comprehensive Stroke Centres in US. Iv rtPA within Golden-3-hours is considered to be the 2nd line treatment, offered only when Neuro-PCI is not available.
|
|
|
|
|
Fig 1 a - g. The procedures of mechanical thrombectomy |
||
| a. Pretreatment angiography shows total occlusion of the M1 segment of the left middle cerebral artery (MCA) (arrow). b and c. Angiogram and illustration of the procedure show the occlusion site and surrounding angioarchitecture. d. Immediate post-procedural angiography shows complete revascularisation (arrow). e. Large syringe is connected to the reperfusion catheter with forceful suction. f. Disrupted clot removed out from body. g. Retrieved whole clot |
The old concept of cerebrovascular accident and the acceptance of the fate of gradual neurological deterioration and the final state of disability, or even death, should have a revolutionary change. The new term "Brain Attack" implies that stroke is not an accident. Just like a heart attack, a stroke is something preventable, treatable, or even curable, without leaving patients with any neurological deficits. Strokes can be tackled in a similar way to heart attacks. In future, patients suffering from acute ischemic strokes will be less miserable. [1,2]
The term "stroke" refers to the sudden onset of neurological impairment due to vascular causes. There are two types of stroke: Ischaemic stroke accounts for ~87% of all strokes in the western world (~70% in Hong Kong). Haemorrhagic stroke explains the remaining 13% (~30% in Hong Kong). Yet haemorrhagic stroke has a higher mortality than the ischaemic entity; it is responsible for more than 30% of all stroke deaths.
Strokes can strike individuals regardless age, race or gender. During ischaemic stroke, a blood vessel in the brain becomes blocked. The blockage disrupts the blood flow, preventing oxygen from being delivered to the area of the brain affected. The section of brain tissue deprived of oxygen becomes "stunned" and no longer functions properly, resulting in the stroke symptoms.
Acute ischaemic stroke (AIS) is a serious medical emergency. Rapid intervention is crucial. For every minute a large vessel stroke goes untreated, as many as 1.9 million neurons are lost (32,000 neurons are lost per second, 120 million neurons are lost per hour), 14 billion synapses are lost , 7.5 miles of myelinated fibers are lost. Permanent neurologic damage is more likely to occur the longer a stroke goes untreated. If treatment is delayed, additional death of critical brain cells occurs "infarction" reducing the potential benefit of the treatment. A short time to treatment is absolutely critical to increase the probability of a good recovery. After approximately three hours, brain cells will suffer irreversible injury usually leading to their death. This is the reason why thrombolytic therapy of rtPA are given only until three hours since the onset of the stroke. Therefore time really is brain.[3]
- Each year roughly there are 18,000 stroke cases in Hong Kong. Each year roughly 795,000 Americans experience a new (610,000) or recurrent (185,000) stroke.
- Stroke is the third leading cause of death in the United States, behind heart disease and cancer. It has been estimated that ~60,000 Americans will die from stroke every year. It causes 10% of deaths worldwide.[4]
- The incidence of stroke is expected to rise in coming decades due to aging populations. It could soon be the most common cause of death worldwide.[5] The incidence of stroke increases exponentially from 30 years of age, and a etiology varies by age.[6]
- Stroke is the leading cause of severe, long-term disability.
- Stroke is the number one cause of inpatient Medicare reimbursement for long-term adult care. Total stroke costs now exceed $63 billion per year in the US. The estimated direct and indirect cost of stroke for 2010 is $73.7 billion.
 |
||
| Fig 2. Total stroke cost in US |
- The personal and financial loss of the more than 3,000,000 people currently living with stroke is enormous.
- Apart from physical and financial burden, stroke also exerts great psychological impact to patients and their family members.
The new concept emphasises screening of stroke risk, the control of risk factors and the prevention on brain attack; public education on stroke symptoms allowing rapid recognition and seeking of emergency help; and, most importantly, fast-track treatment of acute brain attack during the golden hours of the therapeutic window.
Question, Screening, Prevention, Time, Place, Person, 3D8P
(QSP-TPP-3D8P)
1. Question: Ask patients questions: their own estimation of life time stroke risk (reflecting their awareness of own health and family history)
ii. BHCBP Examination: Body Mass Index, Heart status, Carotid artery for bruit, Blood pressure, Pulse for atrial fibrillation.
b. GOCO Laboratory screen: Glucose level, (Oil) Lipid profile, Clotting profile, (Organs) Liver and Renal function.
c. Image screen: Magnetic Resonance Imaging of brain, brain vessels and carotid and vertebral arteries.
(Up to 80% of strokes are preventable; you can prevent a stroke.)
b. POGAS Medical Therapy: Drug for Blood pressure control[11], Cholesterolaemia[11], Glucose control for diabetes[12], Atrial Fibrillation (Anticoagulant)[13], Stroke in the past (Antiplatelet)
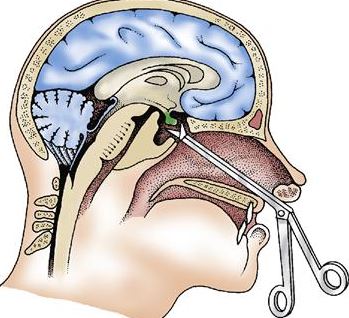
c. Structural abnormalities with or without symptoms: Refer to vascular nerosurgeon for Prophylactic Neurosurgery Percutaneous Cerebral Intervention (Neuro-PCI)
|
|
 |
|
| Fig 3. The Wingspan system of intracranial vascular stent | ||
|
|
||
|
Fig 4a. The Pre-stenting angiogram (DSA) showing right MCA stenosis.
b. stent-in-situ with stent marker (white arrow) c. the post-stenting DSA
|
||
Management of Acute Stroke (TPP-3D8P):
Time--Place--Person--3 Golden hours Drug or PCI—8 Golden Hours only PCI (TPP-3D8P)
1. Time:
b. Promptly seek for emergency help during the Golden-3-Hours therapeutic window.
2. Place: Seek immediate medical assessment and treatment in Hospital equipped with CT scanner, MRI scanner and Angiogram machine.[16]
3. Person: Seek help from vascular neurosurgeon who can provide comprehensive treatment and who can manage the complications associated with ischaemic stroke and its treatment.
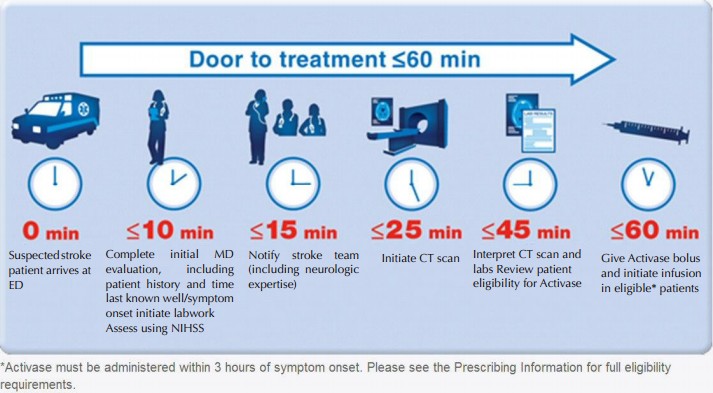
4. 3-Golden-hours Drug or PCI:
b. Most (>90%) of the acute ischaemic stroke patients will not benefit from iv rtPA due to: i. late presentation to emergency room (more than 2 hours after symptom onset), ii. fall into the exclusion criteria of iv rtPA, iii. delayed diagnosis in emergency rooms or clinical wards due to misinterpretation of CT scan.
c. The benefit of iv rTPA should weighted against its associated high risks. Properly informed consent is vital[17,18]
 |
|||
| Fig 5. The Narrow time frame of the iv rtPA Therapy | |||
|
|
|||
 |
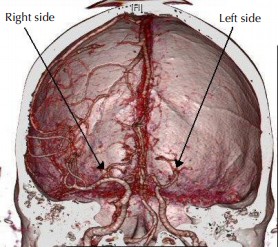 |
 |
|
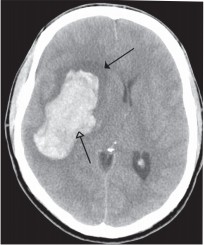
| Fig 6a. Typical dense string sign over Middle Cerebral Artery occlusion (arrow) | Fig 6b. CT angiogram confirm Middle Cerebral Artery occlusion over left side, while right side revealed normal Middle Cerebral Artery | Fig 7. Right capsular intracerebral haemorrhage (arrows) | |
5. 8-Golden-Hours only PCI (Neurosurgical Percutaneous Cerebral Intervention)
b. Intra-arterial fibrinolysis i.e. ia rtPA injected at the site of thrombosis, improves outcomes in acute ischemic stroke.[19]
c. Intra-vascular stent may be deployed if concomitant vascular stenosis exists.
d. Within the Golden-3-hours, Neuro PCI can revascularise the brain cells and minimise the central infarction core. Patients may have full recovery without any neurological deficit.
e. Within the Golden-8-Hours: From the therapeutic window of the 4th hour to the 7th hour, Neuro-PCI revascularisation can salvage brain cells in the peripheral ischaemic region called the Penumbra Zone and minimise the volume of brain infarction. Thus the overall morbidity and mortality of ischaemic stroke is reduced.
f. Neuro-PCI is also indicated for patients who were unable to receive iv rtPA due to contraindications or for whom the drugs were ineffective.[20,21,22,23]
 |
 |
| Fig 8a. The Penumbra System for mechanical thrombectomy | Fig 8b. The Merci Clot retriever for mechanical thrombectomy |
Salvage Neurosurgery
1.Surgery for bleeding complication of iv rtPA
Around 6% of iv rtPA treated patients develop symptomatic intracranial bleeding that cause more disastrous brain damage.[24] Salvage neurosurgery is difficult due to rtPA caused bleeding tendency. Though surgery may be lifesaving, patients may be severely disabled or even vegetative.
 |
||
|
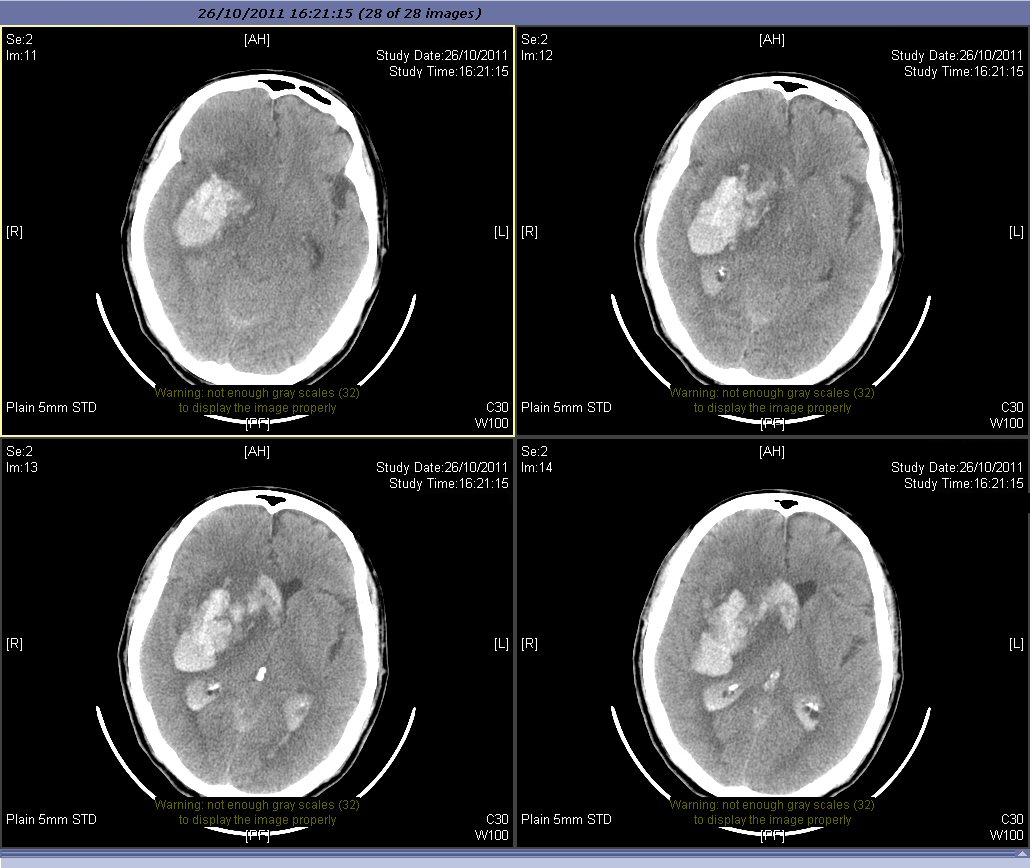
Fig 9a. Severe intracranial bleeding after iv rtPA
|
||
 |
 |
|
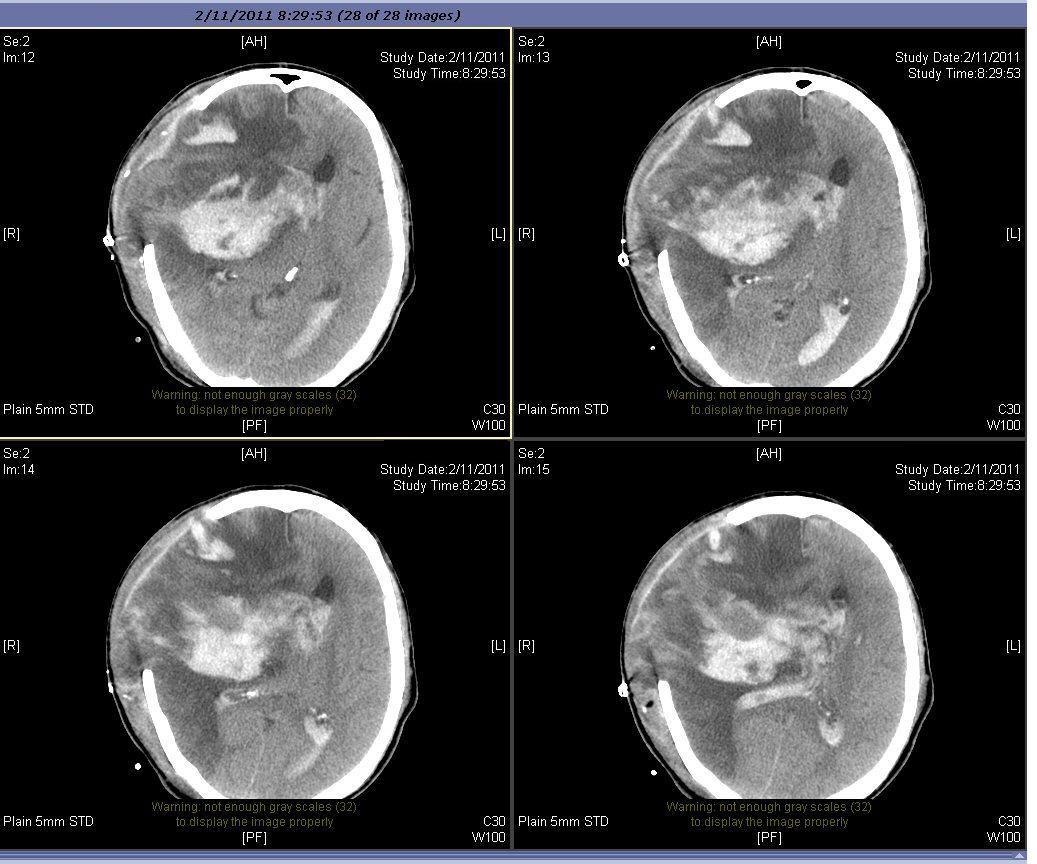
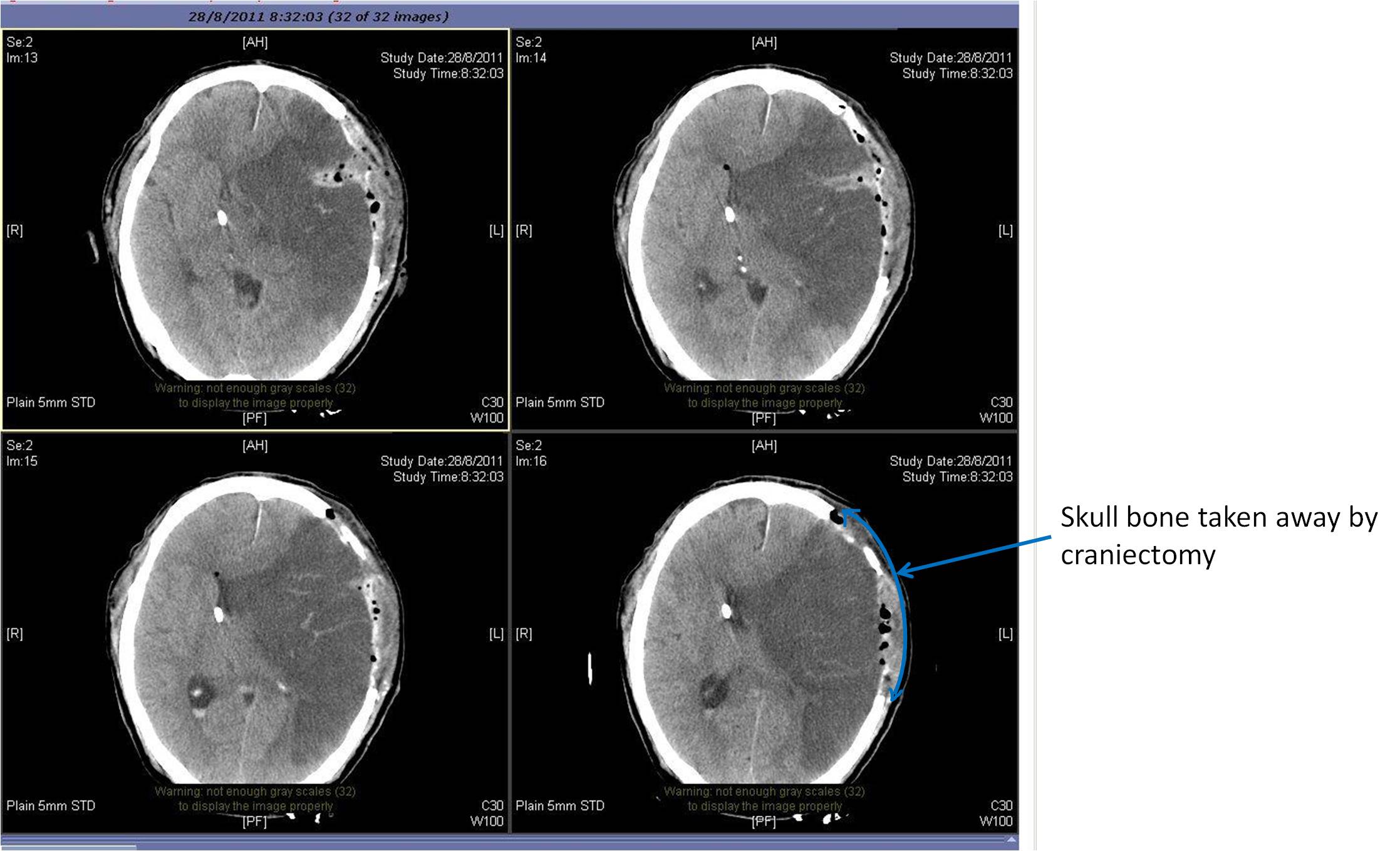
| Fig 9b. After surgery for blood clot removal and craniectomy | Fig 9c. The brain with gross shrinkage | |
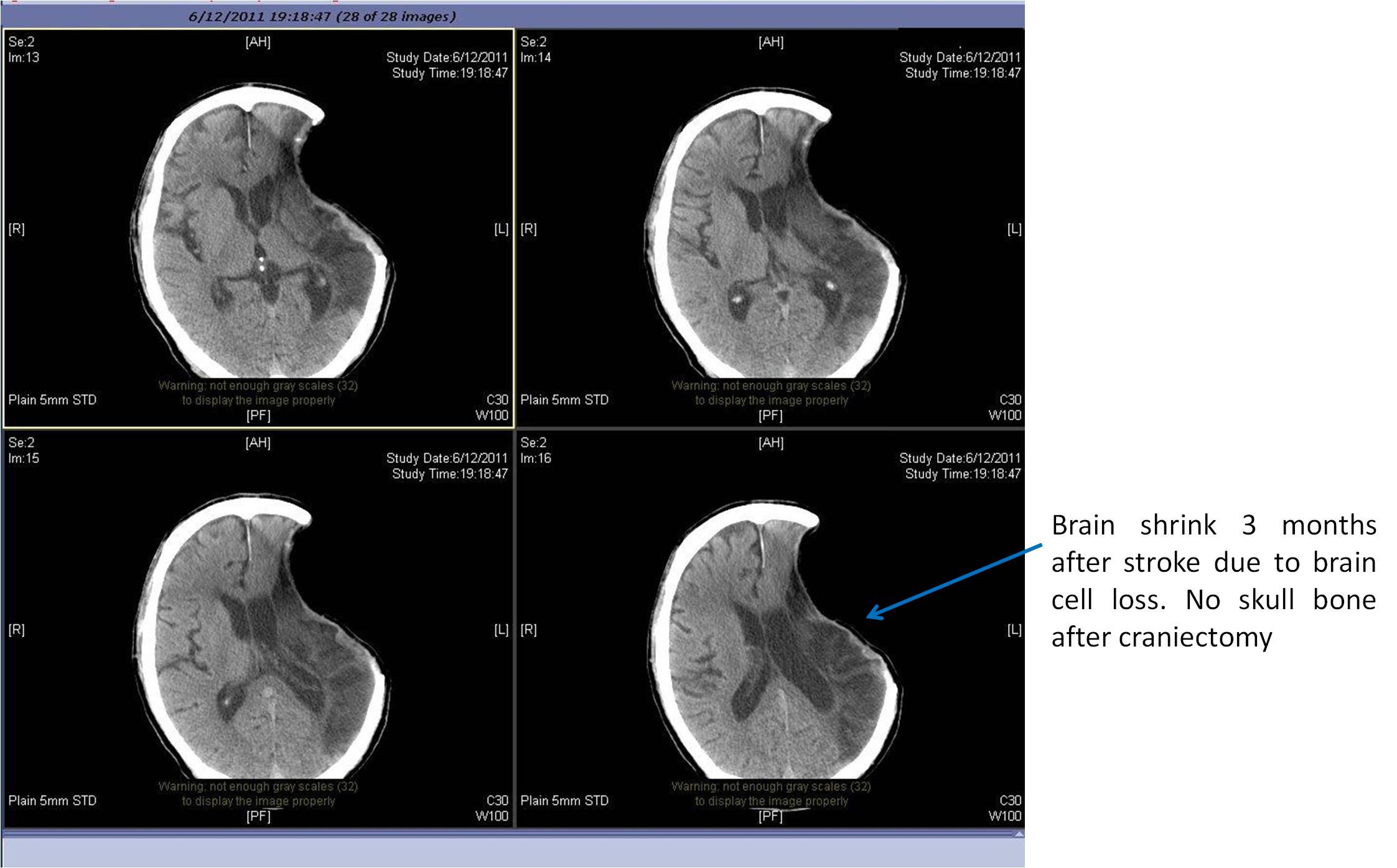
Large territory strokes can cause significant oedema of the brain with secondary brain injury in surrounding tissue. This phenomenon is mainly encountered in strokes of the middle cerebral artery territory, and is also called "malignant cerebral infaction" because it carries a dismal prognosis. Relief of the pressure may be attempted with medication, but some require decompressive craniectomy (temporary surgical removal of the skull) +/- lobectomy with excision of infarcted brain tissue. This confers a marked improvement in the risk of death, although most survivors are disabled.[25]
|
|
|
Fig 10a. Left MCA infarction with mass effect
|
 |
|
Fig 10b. Left sided decompressive craniectomy
|
 |
|
Fig 10c. Finally there is brain shrinkage
|
References
- World Health Organisation (1978). Cerebrovascular Disorders (Offset Publications). Geneva
- Kidwell CS, Warach S (December 2003). "Acute ischemic cerebrovascular syndrome: diagnostic criteria". Stroke 34 (12): 2995–8
- Saver JL (2006). "Time is brain - quantified". Stroke 37 (1): 263–6
- The World health report 2004. Annex Table 2: Deaths by cause, sex and mortality stratum in WHO regions, estimates for 2002. Geneva
- Murray CJ, Lopez AD (1997). "Mortality by cause for eight regions of the world: Global Burden of Disease Study". Lancet 349 (9061): 1269–76.
- Ellekjær, H; Holmen J, Indredavik B, Terent A (November 1, 1997). "Epidemiology of Stroke in Innherred, Norway, 1994 to 1996 : Incidence and 30-Day Case-Fatality Rate". Stroke 28 (11): 2180–2184
- Stroke Risk Factors". American Heart Association. 2007. Retrieved January 22, 2007
- Hankey GJ (August 1999). "Smoking and risk of stroke". Journal of Cardiovascular Risk 6 (4): 207–11
- Gorelick PB (1987). "Alcohol and stroke". Stroke; a Journal of Cerebral Circulation 18 (1): 268–71
- Westover AN, McBride S, Haley RW (April 2007). "Stroke in young adults who abuse amphetamines or cocaine: a population-based study of hospitalized patients". Archives of General Psychiatry 64 (4): 495–502.
- Cholesterol, diastolic blood pressure, and stroke: 13,000 strokes in 450,000 people in 45 prospective cohorts. Prospective studies collaboration". Lancet 346 (8991–8992): 1647–53. 1995
- Dormandy JA, Charbonnel B, Eckland DJ, et al. (2005). "Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial". Lancet 366 (9493): 1279–89.
- Hart RG, Pearce LA, Aguilar MI (2007). "Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation". Ann. Intern. Med. 146 (12): 857–67
- Ederle J, Featherstone RL, Brown MM (2007). Brown, Martin M. ed. "Percutaneous transluminal angioplasty and stenting for carotid artery stenosis". Cochrane Database Syst Rev (4): CD000515
- Derdeyn CP, Chimowitz MI (August 2007). "Angioplasty and Stenting for Atherosclerotic Intracranial Stenosis: Rationale for a Randomized Clinical Trial". Neuroimaging Clin. N. Am. 17 (3): 355–63, viii–ix.
- Donnan GA, Fisher M, Macleod M, Davis SM (May 2008). "Stroke". Lancet 371 (9624): 1612–23
- The National Institute Of Neurological Disorders And Stroke Rt-Pa Stroke Study Group, (1995).
- Wardlaw, JM; Murray, V, Berge, E, Del Zoppo, GJ (2009-10-07). Wardlaw, Joanna M. ed. "Thrombolysis for acute ischaemic stroke". Cochrane database of systematic reviews (Online) (4): CD000213
- Lee M, Hong KS, Saver JL (May 2010). "Efficacy of intra-arterial fibrinolysis for acute ischemic stroke: meta-analysis of randomized controlled trials". Stroke 41 (5): 932–7
- Flint AC, Duckwiler GR, Budzik RF, Liebeskind DS, Smith WS (2007). "Mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and Multi MERCI Part I trials". Stroke 38 (4): 1274–80
- Smith WS, Sung G, Starkman S, et al. (2005). "Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial". Stroke 36 (7): 1432–8
- Lutsep HL, Rymer MM, Nesbit GM (2008). "Vertebrobasilar revascularization rates and outcomes in the MERCI and multi-MERCI trials". J Stroke Cerebrovasc Dis 17 (2): 55–7
- Smith WS (June 1, 2006). "Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part I". AJNR Am J Neuroradiol 27 (6): 1177–82
- Wardlaw, JM; Murray, V, Berge, E, Del Zoppo, GJ (2009-10-07). Wardlaw, Joanna M. ed. "Thrombolysis for acute ischaemic stroke". Cochrane database of systematic reviews (Online) (4): CD000213
- Simard JM, Sahuquillo J, Sheth KN, Kahle KT, Walcott BP (April 2011). "Managing malignant cerebral infarction". Curr Treat Options Neurol 13 (2): 217–29