The Hong Kong Minimally Invasive Brain & Spine Neurosurgery Centre has top specialists who treat complex neurological conditions caused by stroke, tumors, hernias, injuries, and traumas. Each day our skilled neurosurgeons perform dozens of complicated surgeries, saving people’s lives and helping them to restore their health. Thousands of patients go through the doors of our neurosurgery center every year which gives our excellent team of surgeons unparalleled expertise and ability to guarantee exceptional results to all of the patients.
If you are looking for an excellent neurosurgery clinic in Hong Kong, you have come to the right place. Fill in the online form to make an appointment with one of our specialist and start your journey to a healthy and happy life!
Initial stage of treatment is drug therapy for one or two months. The effectiveness of drugs in controlling the pain can help clinical diagnosis. But medications can only be a temporary solution, not a permanent cure for the true cause of trigeminal neuralgia that is: external factors compressing on the nerve and make it short-circuit.
Brain tumors can be subdivided into non-cancerous benign tumor and malignant cancerous tumor. If a tumor is originated within brain compartment ......
Tumors can develop in the vertebrae, nerves, and other tissue throughout your spine. Some spine tumors, such as astrocytomas, occur more commonly in children and adolescents......
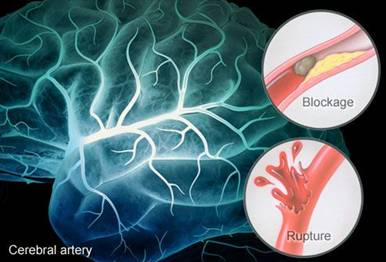
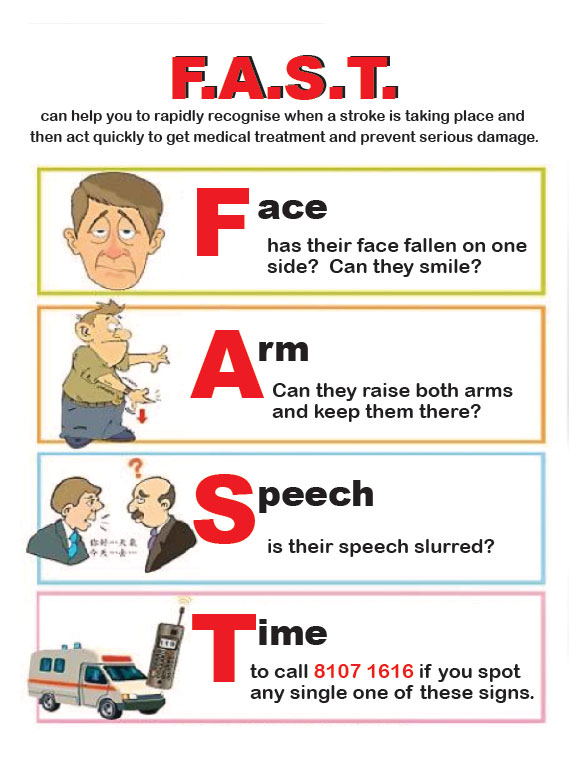
Given the disease burden of strokes, prevention is an important public health concern. As stroke neurosurgeons, we do not want to treat stroke unless we are forced to do so for acute stroke ......
Brain tumors grow and compress normal brain tissue. Both benign and malignant tumors can cause swelling of the brain and raised intracranial pressure. Headache, dizziness....
Since both stroke and heart attack are caused by vascular diseases of various causes. Modern medicine and Stroke Neurosurgeon nowadays consider stroke as ‘brain attack’ its care, either preventive or emergency treatments are similar to that of heart attack.
 |
Given the disease burden of strokes, prevention is an important public health concern. As Stroke Neurosurgeons, we do not want to treat acute stroke, due to much higher risks are involved in emergency settings. However we are forced to do so in order to save lives of patients who are suffering from acute stroke. Actually we want to prevent stroke by promoting stroke risks screening program and stroke prophylactic treatments.
 |
 |
 |
 |
 |
 |
Transient ischemic attack (TIA)
Transient ischemic attack (TIA) is "warning stroke", is the strong predictor of a major stroke. It (TIA) is also often known as "minor stroke" that produce stroke-like symptoms but of no lasting brain damage. It is also caused by a mini-clot that cause transient blockage to blood vessels. As the blockage is transient, unlike a major stroke, there is no permanent damage to the brain. Nevertheless, TIA is an important signal of a major stroke. A person who's had one or more TIAs is almost 10 times more likely to have a stroke than someone of the same age and sex who hasn't. And 1/3 of people with TIAs experience a major stroke in the same year. Therefore recognizing and treating TIAs can reduce your risk of suferring a major stroke. TIA should be considered as medical emergency. It is essential to grasp TIA’s symptoms and followed up immediately with a stroke neurosurgeon, and should be treated in the same way as a stroke.
Lumbar spinal stenosis
Sacroiliac joint pain
Low back pain
Cervical Disc Hernia or Degeneration
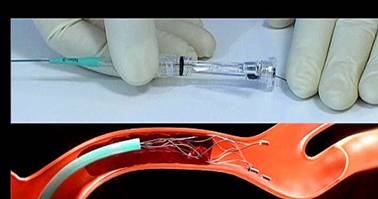
Cervical spine surgery may be indicated for:
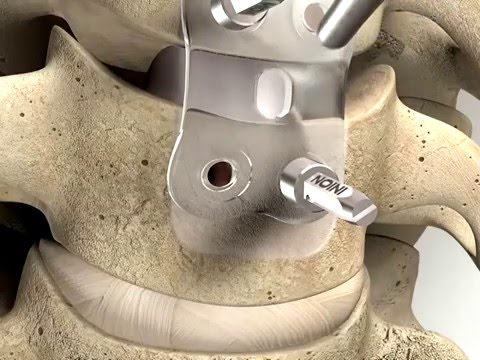
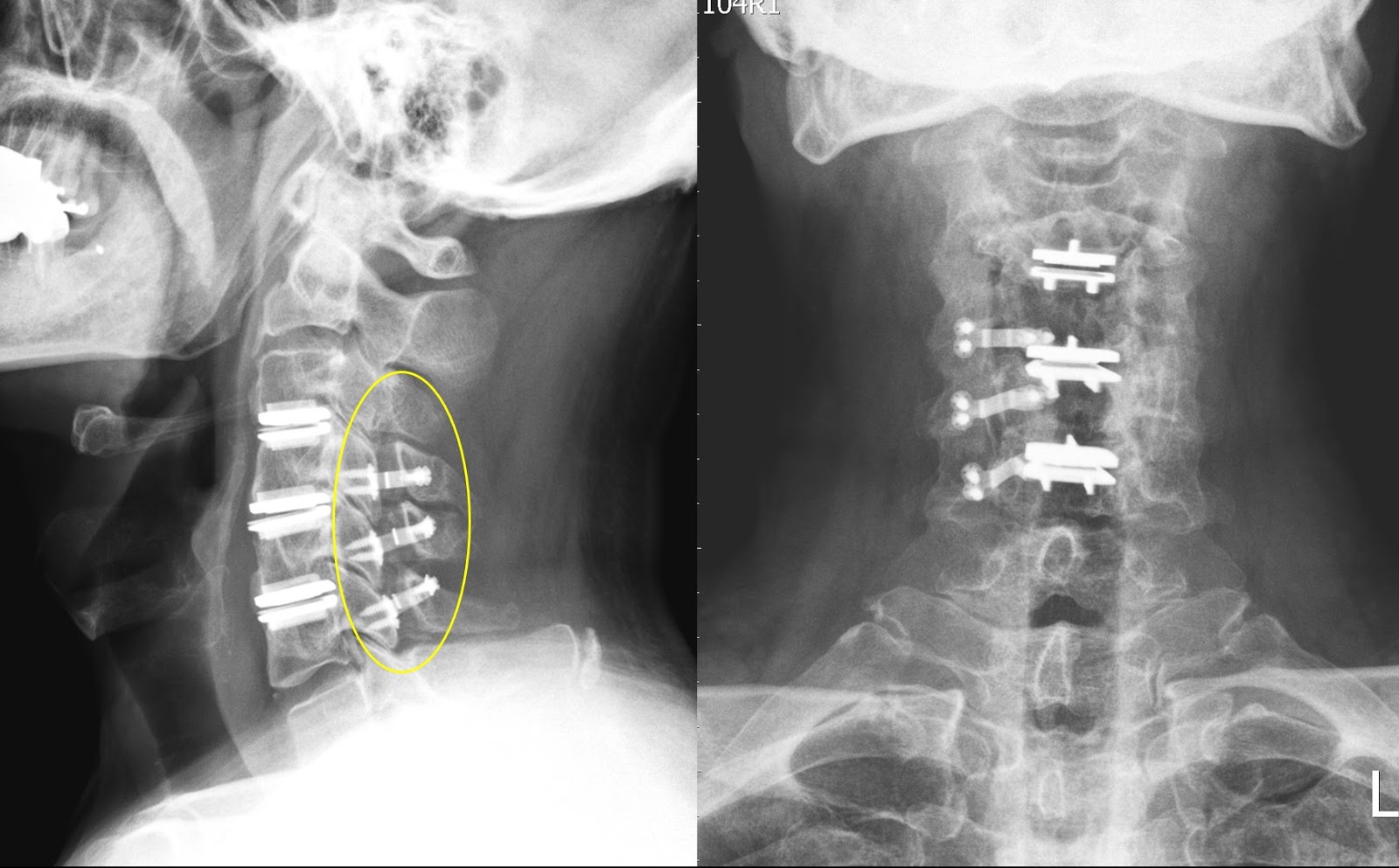
Anterior Cervical Discectomy and Fusion is a common surgical procedure used to treat neck problems such as bulging, herniated disc, degenerative disc disease and spinal instability etc. Discectomy is the removal of the disc and any fragments between the vertebrae. After the disc is removed, the space is filled with a bone graft, the goal is to help the bones to fuse together into one solid bone. This is known as fusion. In order to provide stability during fusion, the doctor may reinforce a metal plate screwed into the vertebrae (cage, screw and plate).The expected outcomes of this operation are to treat for symptoms due to cervical spondylosis aims to relieve pain and prevent further permanent damage to your nerves. Your mobility of neck will be reduced after fixing the disc.
The operation is performed under general anaesthesia. The approach to the cervical spine may vary with individual patient. It can be accessed from the front or from the back. X-ray may be used in the operation room to confirm the level of operation.
After the patient is awaken from the anesthesia, oral feeding may be started. A normal diet may be resumed as instructed after recovery from anaesthesia. Make sure there is no difficulty in swallowing when resuming normal diet. After general anaesthesia, you may experience discomfort in the throat after tracheal intubation. The side effects of anesthesia including feel tired, drowsy, nausea or vomiting. Inform the nurse if symptoms persist or worsen. You should inform the nurse of wound pain. Proper pain relief treatment by injection or oral medication may be prescribed by the doctor.
Patient would be discharge in 1-2 days when the patient can take oral food and pass urine by himself / herself with health condition.
In special patient groups, the actual risk may be different. Other complications may occasionally occur. For further information please contact our spine surgeon.
The intervertebral disc serves to allow flexible movement of human spine and it also acts as a shock absorber or cushion.
It is composed of well-hydrated gel filled nucleus at its central and inner portion (like the same portion of a car’s tyre), and an outer annular fibrous layer (like the rubber outer layer of a tyre. 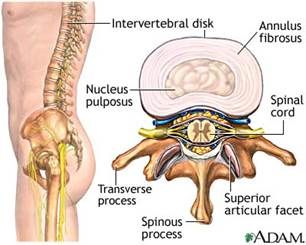
In many ways, the disc analogous to an automobile tyre. As long as the disc remains young, hydrated and being pressurized, it remains strong to support our body weight. A young and healthy disc will be revealed as a White Disc on MRI study of our spine in T2 image. 

However, due to the following reasons:
Our intervertebral disc may become dehydrated (water loss) or dry up at the central gel filled nucleus portion (become a black disc on MRI T2 images), it will depressurizes like to become an old flatten tyre. 
As soon as our disc depressurizes then problems may arise with the increased shear stresses developing on the outer side wall, just as one sees when a car tyre runs flat and fails. After then, depend on individual’s physical heath, various kinds of spine problem begin: 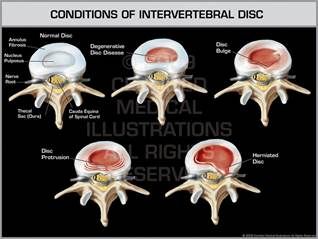

Various kinds of spine symptoms: