The Hong Kong Minimally Invasive Brain & Spine Neurosurgery Centre has top specialists who treat complex neurological conditions caused by stroke, tumors, hernias, injuries, and traumas. Each day our skilled neurosurgeons perform dozens of complicated surgeries, saving people’s lives and helping them to restore their health. Thousands of patients go through the doors of our neurosurgery center every year which gives our excellent team of surgeons unparalleled expertise and ability to guarantee exceptional results to all of the patients.
If you are looking for an excellent neurosurgery clinic in Hong Kong, you have come to the right place. Fill in the online form to make an appointment with one of our specialist and start your journey to a healthy and happy life!
Initial stage of treatment is drug therapy for one or two months. The effectiveness of drugs in controlling the pain can help clinical diagnosis. But medications can only be a temporary solution, not a permanent cure for the true cause of trigeminal neuralgia that is: external factors compressing on the nerve and make it short-circuit.
Brain tumors can be subdivided into non-cancerous benign tumor and malignant cancerous tumor. If a tumor is originated within brain compartment ......
Tumors can develop in the vertebrae, nerves, and other tissue throughout your spine. Some spine tumors, such as astrocytomas, occur more commonly in children and adolescents......
Given the disease burden of strokes, prevention is an important public health concern. As stroke neurosurgeons, we do not want to treat stroke unless we are forced to do so for acute stroke ......
Brain tumors grow and compress normal brain tissue. Both benign and malignant tumors can cause swelling of the brain and raised intracranial pressure. Headache, dizziness....
|
Interventional Pain Management
Pain is a multidimensional experience. Chronic pain differs from acute pain in that it lasts for more than 3-6 months, and there may not be obvious tissue injury leading to the pain. The pathway leading from stimulus to perception may be sensitised [1]. There is often associated depression. Management of chronic pain therefore requires a holistic multi-disciplinary approach [2]. In addition to pharmacological treatment, psychosocial support, physiotherapy and operative treatment, interventional techniques may benefit some patients by defining the pain generator and offers prolonged relief.
Interventional Pain Procedures Commonly performed interventional procedures for pain of spinal origin include trigger point injections, facet blocks, sacroiliac joint blocks, epidural steroids and epidural lysis. Blocks with local anaesthetics identify the source of pain when pain level is reduced significantly after the block. Local administration of steroids decreases inflammation. Denervation by a radiofrequency current can bring prolonged relief by interrupting the sensory pathway. A very small group of selected patients benefits from spinal cord stimulation or insertion of an intra-thecal drug delivery system. Diagnostic blocks with a local anaesthetic help to ascertain the source of pain. Back & Neck Pain Facet joints are small synovial joint connecting the posterior aspects of the vertebrae. Inflammation of these joints or abnormal stress on them can lead to facet joint pain. There are back or neck pain with radiation, but no radicular symptoms. Pain typically worsens on extension. Facet pain syndrome often co-exists with disc pathologies [3]. These joints are supplied by medial branches of adjacent spinal segments. Diagnostic blocks are performed by injection of the joints or the medial branches under fluoroscopy. Joint injections can be supplemented by local steroids. Longer term effect is achieved by radiofrequency lesioning of the medial branches [4,5] (Fig.1).
Sacro-Iliac Joint Pain
Sacroiliac joint pain presents with back pain, usually to the side of lesion, with radiation to the groin or the knee. Bilateral joint involvement may present as central back pain. Interventional treatment approach is similar to facet joint pain [6,7]. More recently developed Cooled Radiofrequency technique produces more consistent lesions for the multiple sacral nerves [8]. Sciatica Radiculopathy presents with back or neck pain with radiation. Lesions in the lumbar levels produce the familiar ‘sciatica’ symptoms, whereas cervical lesions cause pain radiating to the shoulder or upper limb. Radicular pain may be caused by pressure or irritation of the nerve roots by degenerated intervertebral discs. Nerve impingement may also be caused by spinal stenosis, spondylolisthesis or failed back surgery syndrome. Injection of steroids into the epidural space may help these patients. The approaches may be translaminar, transforaminal or caudal [9,10] (Fig. 3). If multiple levels involvement is suspected or for resistant cases, a specially designed Racz catheter can be introduced from the sacral hiatus to define the levels of nerve impingement on epidurogram [11]. Hydrodissection is performed and steroid is deposited [12] (Fig. 4).
Spinal Cord Stimulation
Melzack and Wall proposed the gate-control theory in 1965 [13]. The concept of stimulation of large afferent fibres to close the ‘gate’ for pain perception lead to the development of spinal cord stimulation. Shealy published the application of ‘dorsal column stimulation’ in 1967 [14]. Over the years spinal cord stimulation has developed into a percutaneous technique where a lead with multiple contact points is inserted into the epidural space and is connected to an implanted pulse generator. Programmable electric current stimulates the spinal cord, leading to pain relief. This is particularly useful for very carefully selected patients who suffer from failed back surgery syndrome [15] or arachnoiditi. (Fig.4) Intrathecal Drug Delivery Systems
Implantable intrathecal drug delivery systems are available for delivery of medications such as opioids or baclofen into the subarachnoid space directly. This may be of use for some very selected patients [16]. References
|
|
|
|
|
|
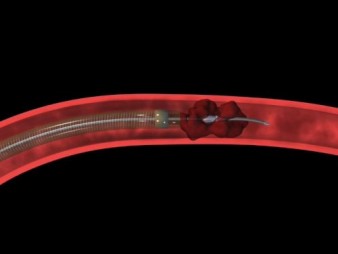
Fig 1 a - g. The procedures of mechanical thrombectomy |
||
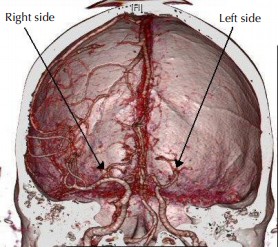
| a. Pretreatment angiography shows total occlusion of the M1 segment of the left middle cerebral artery (MCA) (arrow). b and c. Angiogram and illustration of the procedure show the occlusion site and surrounding angioarchitecture. d. Immediate post-procedural angiography shows complete revascularisation (arrow). e. Large syringe is connected to the reperfusion catheter with forceful suction. f. Disrupted clot removed out from body. g. Retrieved whole clot |
 |
||
| Fig 2. Total stroke cost in US |
|
|
 |
|
| Fig 3. The Wingspan system of intracranial vascular stent | ||
|
|
||
|
Fig 4a. The Pre-stenting angiogram (DSA) showing right MCA stenosis.
b. stent-in-situ with stent marker (white arrow) c. the post-stenting DSA
|
||
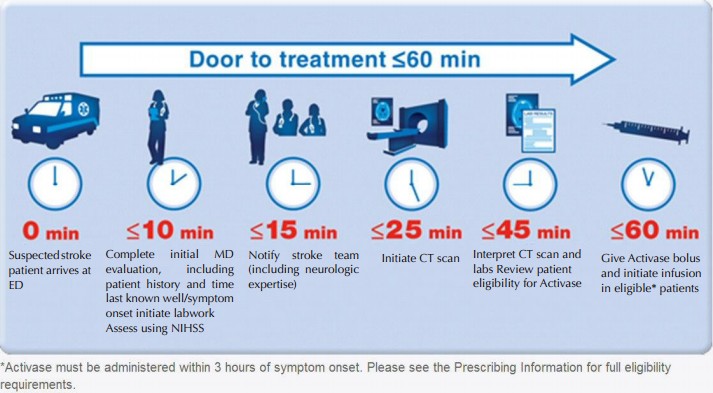
Management of Acute Stroke (TPP-3D8P):
Time--Place--Person--3 Golden hours Drug or PCI—8 Golden Hours only PCI (TPP-3D8P)
1. Time:
b. Promptly seek for emergency help during the Golden-3-Hours therapeutic window.
2. Place: Seek immediate medical assessment and treatment in Hospital equipped with CT scanner, MRI scanner and Angiogram machine.[16]
3. Person: Seek help from vascular neurosurgeon who can provide comprehensive treatment and who can manage the complications associated with ischaemic stroke and its treatment.
4. 3-Golden-hours Drug or PCI:
 |
|||
| Fig 5. The Narrow time frame of the iv rtPA Therapy | |||
|
|
|||
 |
 |
 |
|
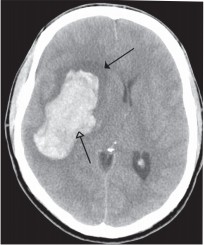
| Fig 6a. Typical dense string sign over Middle Cerebral Artery occlusion (arrow) | Fig 6b. CT angiogram confirm Middle Cerebral Artery occlusion over left side, while right side revealed normal Middle Cerebral Artery | Fig 7. Right capsular intracerebral haemorrhage (arrows) | |
 |
 |
| Fig 8a. The Penumbra System for mechanical thrombectomy | Fig 8b. The Merci Clot retriever for mechanical thrombectomy |
 |
||
|
Fig 9a. Severe intracranial bleeding after iv rtPA
|
||
 |
 |
|
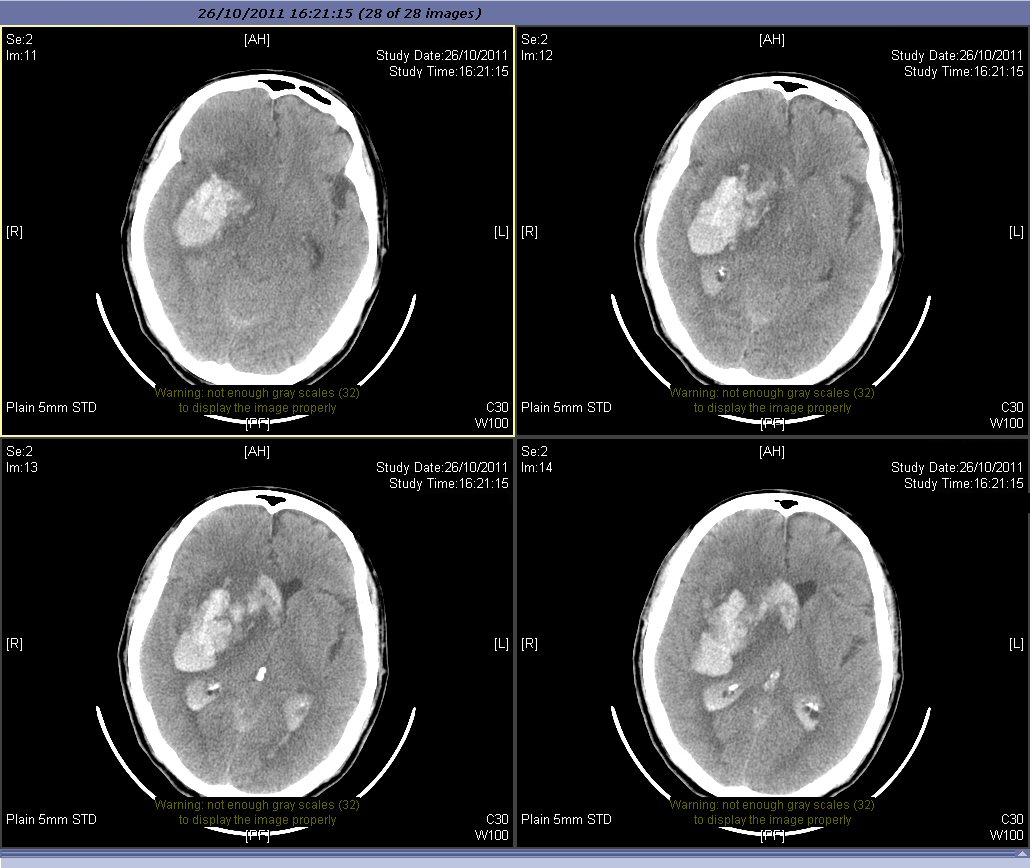
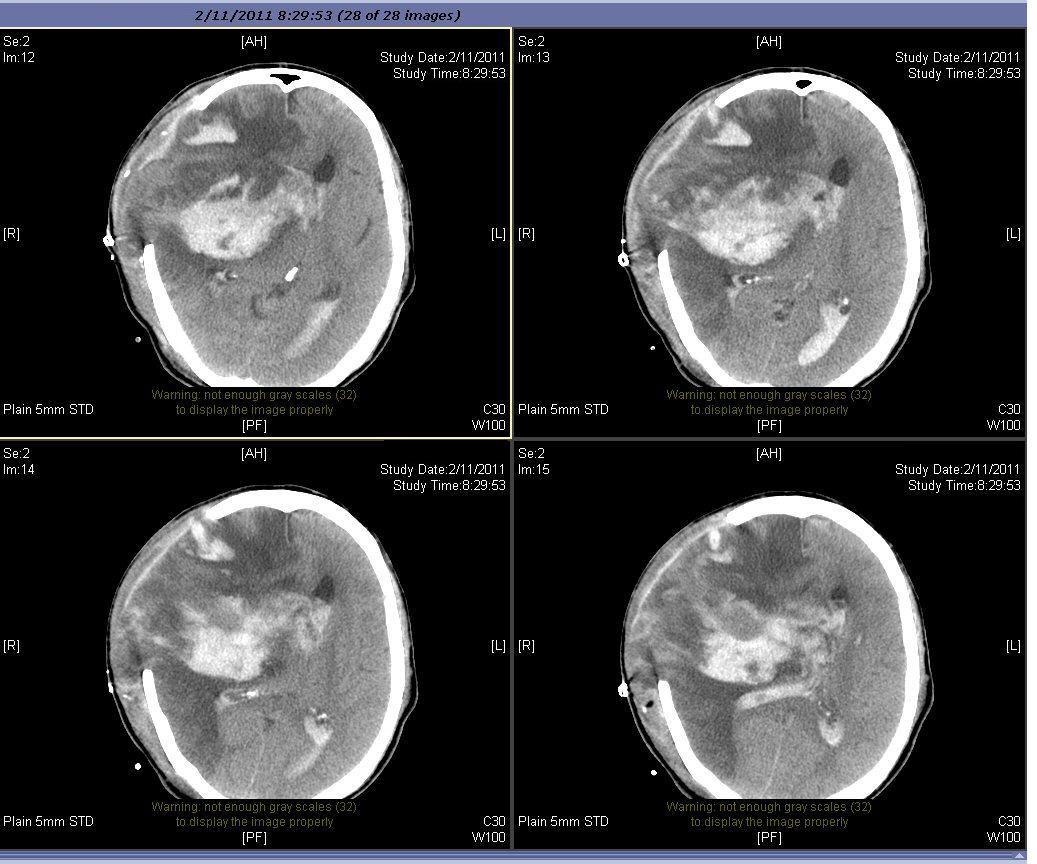
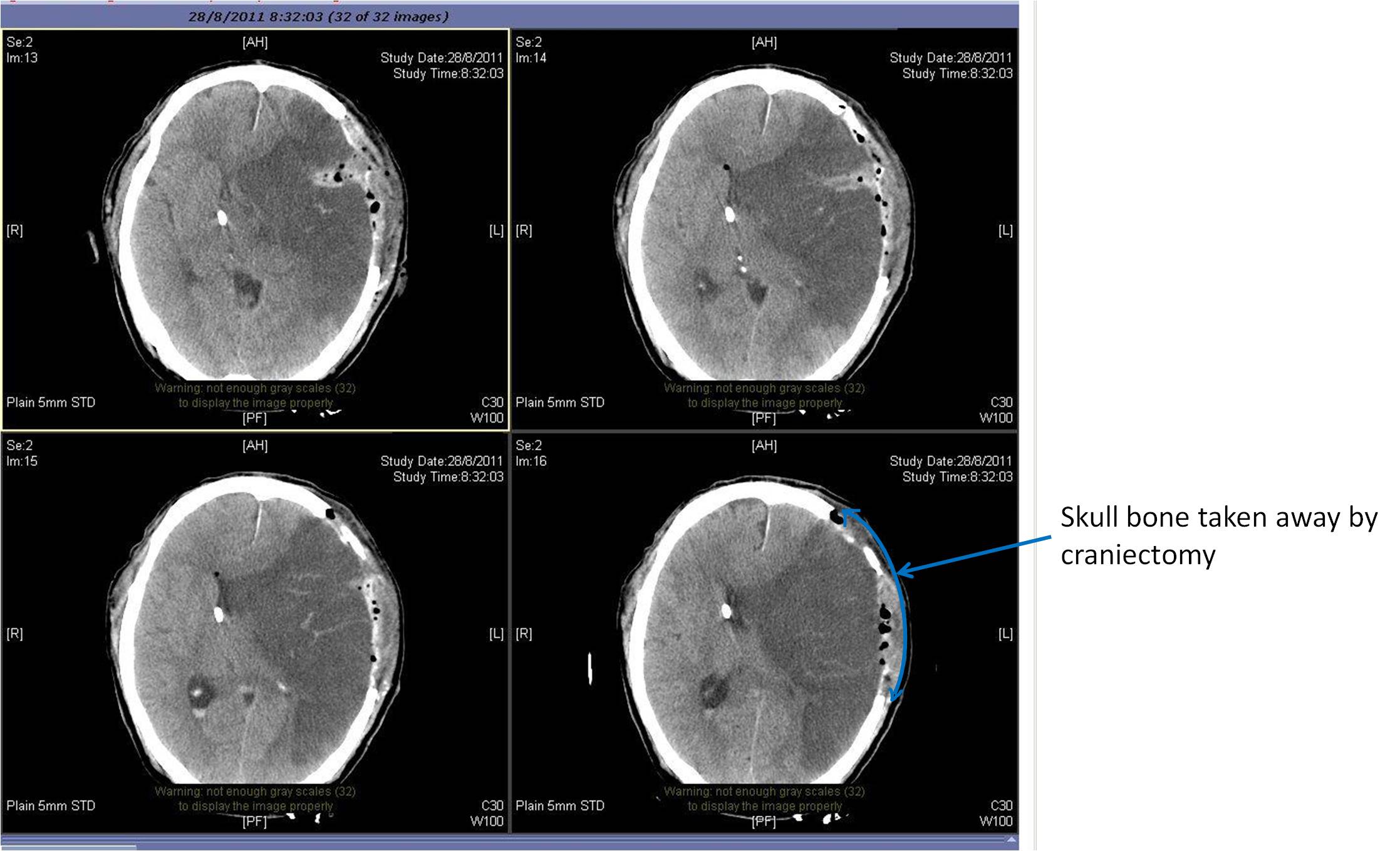
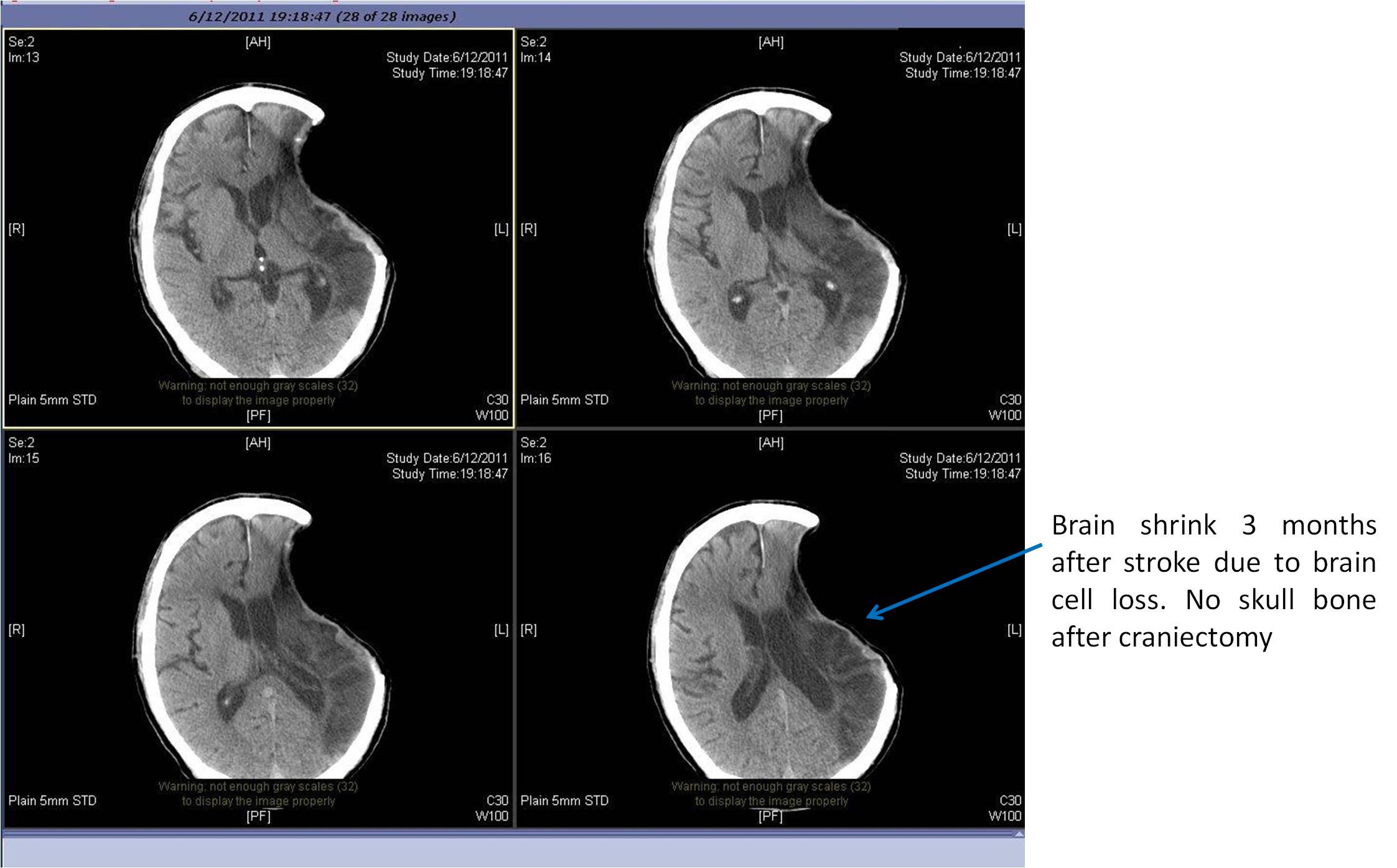
| Fig 9b. After surgery for blood clot removal and craniectomy | Fig 9c. The brain with gross shrinkage | |
|
|
|
Fig 10a. Left MCA infarction with mass effect
|
 |
|
Fig 10b. Left sided decompressive craniectomy
|
 |
|
Fig 10c. Finally there is brain shrinkage
|
References
Yes, only if stroke being treated within right time within Golden-Hours before permanent brain damage occurs. All neurological deficits may be reverted normal if stroke patient being treated within right time (within Golden Hours) at right hospital (equipped with stroke services & instruments) by right person (Stroke Specialists).
Type of emergency treatments: An ischemic stroke is occasionally treated in a hospital with thrombolysis (also known as a "clot buster"), and some hemorrhagic strokes benefit from neurosurgery
Intra-venous i.v. thrombolysis with recombinant tissue plasminogen activator (rtPA) in acute ischemic stroke, when given before three to four and a half hours of symptom onset, in long term improves the rate of functional independence among stroke survivors. However most of the stroke patients are not eligible or cannot receive the treatments within 3-4.5 hours. Besides, there are many contraindications (such as abnormal lab values, high blood pressure, or recent surgery) to be considered before the drug is administered. Moreover, the treatments regimen based on a plain CT brain image for clinical decision, with or without a detailed angiogram mapping of neck and brain vessels to look for the exact cause of stroke, rtPA thus carries 6.4% risk of causing substantial brain hemorrhage leading to severe morbidity and mortality.
Under X ray control, a stroke neurosurgeon can pass a very fine catheter up to carotid artery at neck or into the brain arteries. The procedure allows removing obstructing blood clot and offer an option for those who either are not eligible for or do not improve with intravenous thrombolytics of Golden 3-4.5 hours treatments. Our clinical experience observed complete reversible of all neurological deficits for some patients if early artery unblockage were performed within 8 hours after symptom onset. Some patients with good collateral blood supply to brain may allow their brain to withstand or tolerate an even longer golden hours of therapeutic window. Similar to Golden 3-4.5 Hours Treatments, medical literatures reviewed that significant complications occur in about 7% of cases.